DIGESTIVE TRACT – THE BASICS
Before jumping into the Histology of the Digestive Tract let’s get into the basics of it.
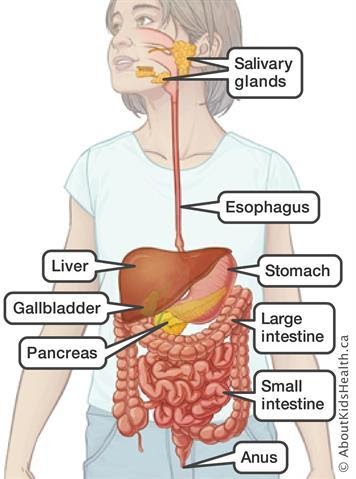
• What is a digestive tract?
It includes the oral cavity, oesophagus, stomach, small and large intestine and anus.
Glands situated with it: salivary glands, pancreas and liver.
It is also called gastrointestinal tract.
• What is the function of the GI tract?
To obtain the molecule from ingested food for maintenance, growth and energy needs of the body.
It allows :
- Ingestion – Introduction of food and liquid into the oral cavity.
- Mastication / Chewing – Breaking solid food into digestible pieces.
- Motility – Muscular movements of materials through the tract.
- Secretion – Secrete lubricating and protective mucus, digestible enzymes, acidic and alkaline fluids and bile.
- Hormonal release –Release hormone for local control of motility and secretion.
- Chemical Digestion / Enzymatic Degradation – Breaking large macromolecules into small by enzymes.
- Absorption – of small molecules into blood and lymph.
- Elimination – eliminate indigestible, unabsorbed components of food.
• Describe the walls of the GI Tract?
It has 4 layers –
- Mucosa:
a) Epithelial Lining
b) Lamina Propria ( underlying layer of loose connective tissue rich in blood vessels, lymphatics, lymphocytes, smooth muscle cells, often containing small glands).
c) Muscularis Mucosae ( thin layer of smooth muscles which separates mucosa from submucosa and allowing local movement of mucosa. It is also known as mucous membrane).
2. Submucosa : It contains dense connective tissues with larger blood and lymph vessels and the Submucosal plexus / Miessner plexus of autonomic nerves, glands and significant lymphatic tissue.
3. Muscularis / Muscularis Externa : It is thick
* Composed of 2 layers of smooth muscle cells
* Internal sublayer – lies closer to lumen with circular fibre orientation.
* External sublayer – lies away from lumen with longitudinal fibre orientation.
* Connective tissue between these sublayers contain blood, lymphatic vessels and Myenteric / Auerbach nerve plexus( they mix and propel luminal contents forward by contraction) of many autonomic neurons aggregated into small ganglia and interconnected by pre and post ganglia nerve fibres.
Myenteric Plexus and Missener Plexus forms Enteric Nervous System
- Serosa : Thin layer of loose connective tissue.
- It is rich in blood vessels, lymphatics and adipose tissue with a simple squamous covering epithelium (mesothelium).
- In the abdominal cavity, serosa is continued with mesenteries (thin membrane covered by mesothelium on both sides that support intestine) and they continue with peritoneum ( serous membrane that lines the cavity).
- In place, where GI tract is not suspended into cavity but bound directly to adjacent structure serosa is replaced by thick adventitia ( connective tissue layer that merges with surrounding tissues and lack mesothelium)
Numerous free immune cells and lymphoid nodules in mucosa and submucosa constitute MALT ( mucosa associated lymphoid tissues )
HIRSCHSPRUNG ( Congenital Aganglionic Megacolon ) or CHAGAS DISEASE ( Trypanosomiasis ) : Plexus in digestive tract’s enteric nervous system are absent or severely injured respectively and produce dilation in some areas.
LAYERS OF GI TRACT

For more information Visit Our Site
To submit your work Contact US






